Preterm infants often experience delayed oral feeding skills due to difficulty coordinating an appropriate suck-swallow-breathe pattern; it’s this pattern that leads to the achievement of full oral feedings.1 The extent of prematurity, severity of illness and the number of medical interventions are positively correlated with a delay in acquisition of eating skills2 and increased risk of needing a G-tube placed at discharge.3 Failure to achieve full oral feedings in a timely manner contributes to many short- and long-term complications to the infant, caregivers and healthcare system.4
Developmental impacts
Caregiver stress

Increased stress before and after NICU discharge can occur due to their infant’s lack of feeding abilities and difficulties learning their infant’s feeding cues.5
Ongoing feeding challenges
Up to
42%
of preterm infants experience feeding problems in the first four years of life.6
35%
of preterm infants are more likely to have total feeding problems.7

29%
are more likely to have refusal or picky eating.7

34%
have oral motor problems compared to full term infants.7

Adverse neurological outcomes

Feeding difficulties have the potential to serve as an early marker for brain alterations associated with atypical motor and neurological development.
40%
Preterm infants with feeding difficulties are 40% more likely to be diagnosed with a developmental coordination disorder (DCD) at 4‑5 years of age, compared to infants without feeding issues.8

Neurodevelopmental delays

+37%
Preterm infants who do not achieve full oral feedings by 40 weeks post-menstrual age (PMA) are at a 37% increased risk of having adverse neurodevelopmental outcomes, such as lower cognitive, language and motor scores at 18-26 months.9
Simply requiring a G-tube at discharge is a predictor of a preterm infant’s future neurodevelopmental delay.10 Infants discharged on a G-tube had lower cognitive communication and motor composite scores.10

Clinical and financial impacts
Prolonged dependency on tube feeding
50%
of infants born at or earlier than 28 weeks were likely to still need a G-tube upon discharge,

25%
compared to 25% of infants born between 28-32 weeks.3

Poor nutritional status

Infants with feeding problems have a higher risk of nutritional deficiencies, regardless of whether they have G-tubes.12
Length of stay

Delays in adequate oral feeding increase the time that premature infants remain hospitalized.11
37%
A large, multi-center NIH study found that inadequate oral feeding is the most common barrier to discharge in moderately preterm infants, affecting 37% of infants who remained hospitalized at 36 weeks PMA.11

Growth failure

Poor nutritional status in preterm infants, as a result of delayed feeding, increases the risks of growth failure.12
11%
In a study published by the Journal of Pediatrics, 11% of preterm infants with G-tubes had birth weights that were small for their gestational age.12

56%
of infants with G-tubes had weight that fell into the <10th percentile.12

Preterm birth costs

Preterm birth healthcare costs in the U.S. are estimated to be more than
$26 billion/year
13
Variability in approaches to feeding preterm infants likely contributes to this high cost.12
Standardizing feeding development
The development of non-nutritive sucking (NNS) skills is an essential precursor for infants to achieve their independent oral feeding milestones and often the last criterion for NICU discharge.
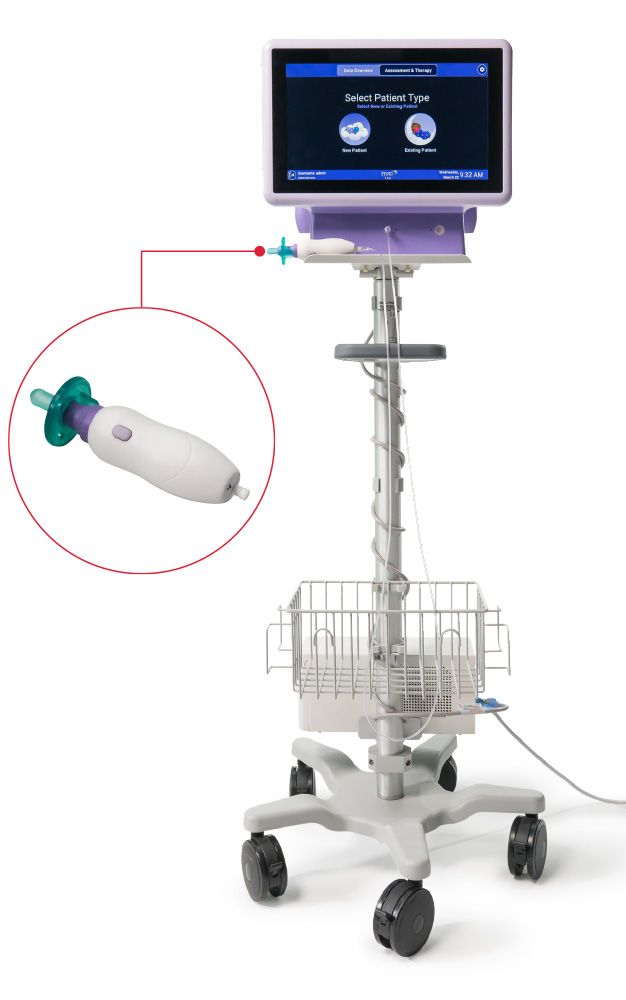
The Cardinal Health™ Kangaroo NTrainer™ System is the only FDA Class ll biofeedback device designed to help newborns and premature infants develop the non-nutritive sucking skills needed to transition to independent oral feeding.
Through real-time assessment technology and therapy delivery, the NTrainer™ System can accurately show, based on objective criteria (i.e., strength and pattern of suck), a baby’s progress toward readiness for oral feeds. This can help clinicians more easily recognize an infants’ readiness to transition to breast or bottle, thus helping to reduce NICU length of stay14 and reach short-term developmental milestones. It can also reassure parents and other caregivers of their baby’s developmental progress.15